Health Equity
CalPERS is committed to ensuring exceptional health care and equitable health outcomes for all members and their beneficiaries, regardless of race, ethnicity, preferred language, sexual orientation, or gender identity.
CalPERS recognizes that addressing health disparities requires alignment with other large purchasers and statewide organizations, commitment, focus, and accountability to create meaningful change.
To this end, we created the Health Demographic Profile (HDP) in our myCalPERS member self-service portal, which allows health members to self-report their race, ethnicity, preferred language, sexual orientation, and gender identity.
We’re using their responses to see if health outcomes, member experience of care, or preventive care differ based on a member’s demographics. The information from the HDP will be used to direct programs, policies, and interventions on behalf of our members.
Key Highlights
- Hired a health equity officer to lead a coordinated, cross-divisional effort for all things health equity.
- Executed a multi-pronged communication plan to educate members about the importance of health equity. This included a designated website landing page, video, and presentations to employer groups, state employee groups, and retirees.
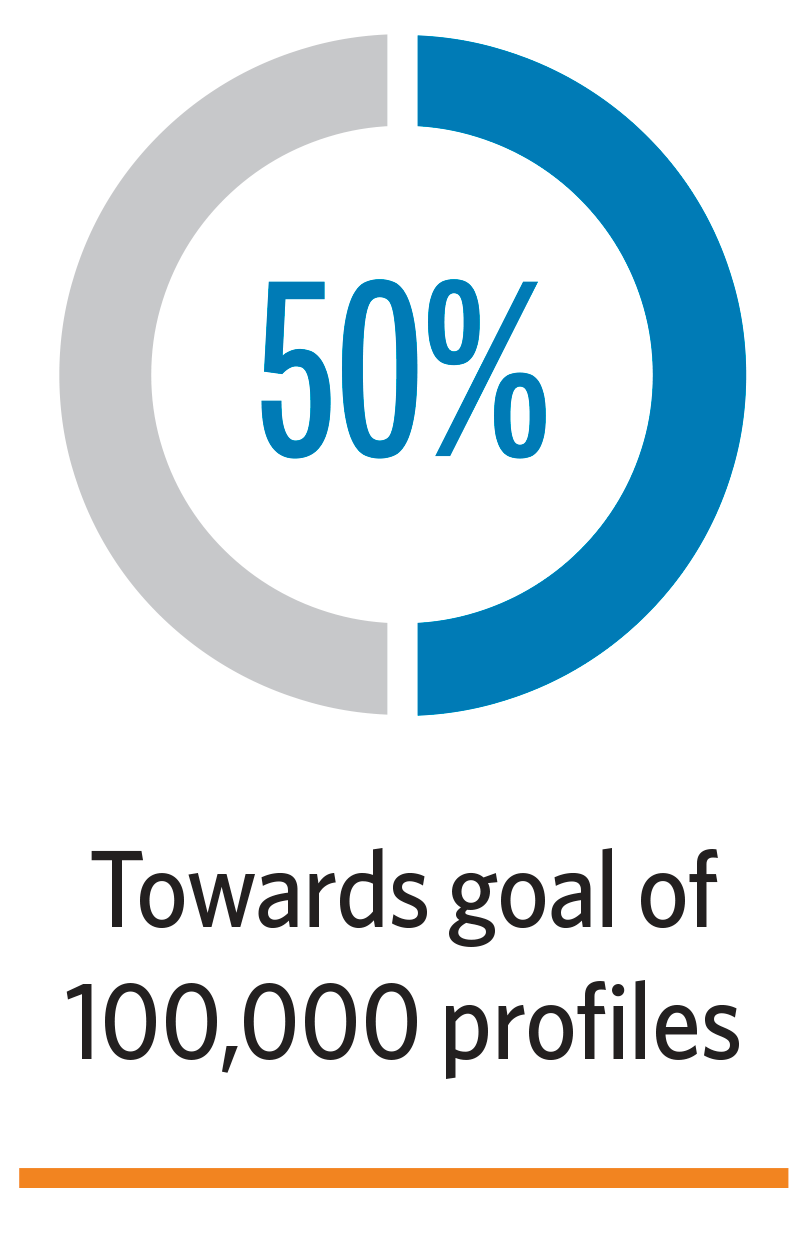
- Continued work to reach 100,000 completed profiles through myCalPERS HDP, CalPERS will begin evaluating clinical quality measures for colorectal cancer screening, breast cancer screening, and comprehensive diabetes care HbA1c control. As of June 30, more than 50,000 profiles were created, moving CalPERS halfway toward our goal of 100,000 profiles. Collected health demographic data for health plan grievance and appeals cases. We also began to analyze data to identify trends and whether healthcare access or quality of care disparities exist.
- Executed a health demographic profile awareness campaign which included emails, blogs/newsletters, a dedicated webpage, digital ads, myCalPERS banners, and video.
- Utilized the 2021 Open Enrollment period to promote the HDP via the open enrollment newsletter, emails, and the PERSpective blog.
- Conducted proactive outreach and presentations to large employers, retirees, labor groups, and state agencies to promote completion of the HDP and educate groups on the importance of health equity and data collection.
- Promoted the generation of new ideas to increase the number of health demographic profiles through the Emerging Leader and CalPERS health academy programs.
Conducted focus groups and launched a Behavioral Health Access Survey to collect health demographic data to identify disparities in behavioral health care among CalPERS members in collaboration with University of California researchers. The project began with the compilation of current research, a review of existing benefits, and an evaluation of the annual Member Health Survey.
Added a new strategic measure to the 2022-2027 Strategic Plan that focuses on health equity and utilizes a Health Equity Index (HEI). The HEI includes milestones that foster health equity by creating a consistent infrastructure for improving outcomes, narrowing health disparities, and creating a culture of health equity for CalPERS members.
- Analyzed health benefits and recent grievance and appeals data to identify disparities in care quality or access to create a more equitable benefit structure.
- Identified areas for improvement related to hearing aid benefits, reproductive health, and infertility benefits.
- Changed our definition of infertility to ensure timely access to infertility treatments to members regardless of their age, sexual orientation, gender identity, or marital status.
- Updated the Reproductive Health Services benefit language to ensure members had timely access to reproductive health benefits regardless of gender, sexual orientation, or gender identity.
- Amended the hearing aid benefit to cover 100% of the cost for both ears every 36 months when medically necessary to prevent and treat speech and language development delay due to hearing loss.
- Confirmed that Preferred Provider Organization Health Plans will implement matching their members with a primary care provider to ensure high-quality and more equitable care. Primary care teams play a critical role in preventing and controlling common chronic diseases, addressing social determinants of health and health disparities, and coordinating testing and specialist care when needed.
- Coordinated with health plans on the implementation and communication of benefit design changes to members prior to the 2021 Open Enrollment period.
Continued engagement with the Joint Purchasers Clinical Forum workgroup to increase access, address inequities, and improve quality of health care at an affordable cost. The workgroup is comprised of large healthcare purchasers, including Covered California, Department of Health Care Services, Department of Managed Health Care, and health plan providers, whose work has the potential to impact not only CalPERS health plan members but all Californians.
The following changes were adopted in 2021-2022 related to health plan contract implementation and are part of a continuous effort to improve health equity:
- Standards to address health care gaps created by the COVID-19 pandemic; inclusion of childhood immunization status; and addition of colorectal cancer screening.
- Requirement that health plans work to attain the National Committee for Quality Assurance (NCQA) Multicultural Health Care Distinction for 2022, and report on cultural needs of members and culturally appropriate access to care. This requirement helps the health plans create an actionable health equity framework within their organizations to identify and eliminate health disparities within their membership.
- Requirements for health plans to collect and report self-reported members by race/ethnicity information. This requirement helps plans create a data-informed foundation for health equity and disparities reduction.
- Provided recommendations about the quality of California’s managed care health plans and equity standards to the Director of the Department of Managed Health Care (DMHC) as part of the committee.
- CalPERS’ Chief Clinical Director is a non-voting member of the committee and provides her expertise to the committee.
- Provided committee with recommendations of health plan standards. The DMHC will establish health plan data collection and reporting standards effective 2023 and health equity and quality benchmarks by 2026.